PCOS - Made Simple
Dr. A. NARUMALAR, MS, DGO.
Vijay Nursing Home
Madurai-9
PCOS - Most Common Endocrine Disorder
•Probably the most common endocrine disorder in women of reproductive age
•Prevalence: 8 % to 18 %
•ADA - 2016 - PCOS - Metabolic reproductive syndrome
1990 NIH Criteria (all 3 must be met)
•1. Hyperandrogenism either clinical or bio chemical
•2. Menstrual irregularity (oligo - or an ovulation)
•3. Polycystic Ovaries
Loading…
Exclusion of other causes
•Prolactinoma
•Thyroid disease
•Virilizing tumors of adrenal or Ovarian tumors
• Congenital adrenal hyperplasia
•Cushing’s syndrome
2003 Rotterdam Criteria
•Presence of atleast two of the following:
•Oligo / anovulation
•Hyperandrogenism
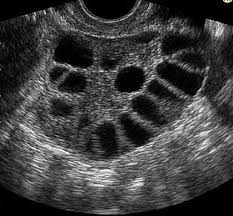
•Polycystic Ovaries on ultra Sound
•And the exclusion of other causes.
3. 17 (OH) Progesterone < 200 ng/dl - rules out NCCAH (21 Hydroxylase deficiency
•Total testosterone > 150 ng/dl - Suggestive of adrenal or Ovarian androgen secreting tumor
•Dexamethasone suppression test - T. Dexamethosone, 1mg given at bed time and plasma cortisol measured the next morning >130 n mol/It - Cushing’s syndrome
- Autosomal dominant inherited factor
• CYP21 gene mutation has been discovered
• Familial occurrence
• Genetic post receptor defect is unique to PCOS
• 80% obese PCOS
• 30 % - 40% lean PCOS
• In utero malnutrition results in IUGR baby which later develops PCOD
Loading…
Development of PCOS and its sequelae
Insulin Resistance
•It is decreased responsiveness of target tissues (muscle, fat, liver) to normal circulating insulin
•Homeostasis model assessment – insulin resistance (HOMA IR)
Fasting plasma insulin U / ml X Fasting plasma glucose m mole / litre
22.5
Normal: 2.1 – 2.7
IGT: 4.3 – 5.2
T2DM: 8.3 – 9.5
Causes of insulin resistance
•Genetic
•Acquired – Ageing, Antenatal, Excess Fat, Emotional Stress, Inactivity, ingestion of drugs, smoking, obesity, urbanisation, uterine mal nourishment
Mechanism
•Mutant insulins
•Insulin antagonist in circulation ( free fatty acids, antibodies, hormones, cytokines)
•Insulin receptor abnormality
•Post receptor defects
-
PCOS - Manifestations - Endocrinological Changes
• Oestrone / E2 level rises
• LH Level is raised over 10 iu/ml
• FSH level remains normal, but FSH/LH ratio falls
• SHBG level falls due to hyperandrogenism
• Testosterone and epiandrostendione levels rise
• Testosterone>2ng / ml, free T>2.2pg / ml (Normal level 0.2-0.8 ng / ml)
• Normal androstenedione level is 1.3-1.5 ng / ml
• DHEA> 700 ng/ml suggests adrenal tumour.
• Prolactin is mildly raised in 15% cases
• Fasting insulin is more than 10 mIU / I in PCOS
• Thyroid function tests may be abnormal (hypothyroidism)
Metabolic Abnormalities:
•OGTT – consisting of fasting and 2 hour glucose using a 75 gram oral glucose load to screen impaired glucose tolerance and T2DM in adolescence and adult women in PCOS because they are at risk
•HBA1C
•Rescreening suggested every 3 to 5 years or more frequently if clinical factors such as central adiposity, substantial weight gain and / or symptoms of diabetes develop, cardiovascular risk
•Lipid profile
Loading…
GOALS:
•Amelioration of hyper androgenic symptoms (hirsutism, acne, scalp hair loss)
•Management of underlying metabolic abnormalities and reduction of risk factors for Type II Diabetes and Cardiovascular disease
•Prevention of endometrial hyperplasia and carcinoma
•Contraception for those not pursuing pregnancy
•Ovulation induction for those pursuing pregnancy
8. Treatment
- Lifestyle modification
- Insulin lowering agents
- Androgen suppression
- Anti - Androgens
- Progesterone +Estrogen
- Ovulation Induction.
Lifestyle Modification
•Diet – avoid junk foods
Plenty of vegetables, fruits
•Exercise – 30 minutes of exercise 5 times in a week
•Stop smoking
Insulin Sensitisers
•Metformin – treat the root cause of PCOS
•Rectify endocrine and metabolic function
•Improve fertility rate
•Does not cause hypoglycemea
•C/I hepatic and renal disease
•Dose 1-1.5 gm / day
Role of Metformin
Endocrine Society Guidelines 2013
•The use of Metformin as a first line treatment of cutaneous manifestations for prevention of pregnancy complications, or for the treatment of obesity has no longer been suggested
•Metformin is suggested in women with PCOS who have T2DM or IGT, who fail lifestyle modification
•Metformin can be considered as a second line therapy for women with PCOS and menstrual irregularity who cannot take or do hot tolerate HCS
•Metformin can be considered as an adjuvant therapy for infertility too
•Use of Metformin to improve reproductive outcomes in PCOS in limited – Cochrane database 2009
Progesterone
Estrogen + Progesterone
•Regular with drawal bleeding
•Reduction in the risk of endometrial hyperplasia or cancer because
•Reduction in LH Secretion and reduction of ovarian androgens
•Increased sex hormone binding globulin production and consequent
•Improvement in hirsutism and acne
of progestin opposition of estrogen
reduction in free testosterone
Role of Hormonal contraceptives (HC s)
HC s (ie., oral contraceptives, patch, or vaginal ring) are recommended as first line management for the menstrual abnormalities and hirsutism / acne of PCOS, which can treat these two problems concurrently
Women with PCOS have a very high incidence of pregnancy loss (30% - 50%)
•Insulin resistance underlies the pregnancy loss (Glycodelins:
•Insulin sensitizers reduce the risk of pregnancy loss
•No evidence that insulin sensitizers should be continued past the first trimester
Endometrial proteins should be low to favour implantation)
Anti androgens
•(i) Spironolactone and (ii) Cyproterone acetate
•Spironolactone in a dose of 100-200 mg daily blocks the androgen receptors, reduces its production and increase its metabolism, and thus prevents further hirsutism in 60% cases
•The side effects include a transient diuresis, menstrual irregularity (Polymenorrhagia 10%) and breast enlargement. Occasionally hyperkaliemia and hyponatremia may occur
•Cyproterone acetate is a potent progestogen, a synthetic derivative of 17 alpha-hydroxyprogesterone; it inhibits DHT binding to its receptors at the periphery and has weak corticosteroid effect. It is given combined with oestrogen as 50 - 100 mg cyproterone daily for the first 10 days of the menstrual cycle with 30 - 50 ug of ethinyloestradiol (EE) for 21 days
•Drospirenone 3mg with 30 ug oestradiol (Yasmin, Janya , Tarana) used cyclically for 3 weeks is found very effective in hirsutism in PCOD
Myo - inositol (MI) and D - Chiro - inositol (DC)
• Inositols are Sugar Alcohols (Alcohol of Cyclohecance)
• Exists in 9 forms (Stereo - isomers)
• Most prominent form is Myo - Inositol
MI
• Can be produced in human body by Glucose
• Once considered a member of the Vitamin B complex (formerly Vitamin B8
• It is an insulin sensitizer, and second messenger of the insulin signaling
DCI
• One of the 9 isomers of Myo - Inositol
• Normal Physiological ratio MI : DCI = 40 : 1
• Peripheral action (Outside Ovaries)
•Normally in the body 100 : 1 in PCOS it is 0.2:1
•Myo inositol is a Valuable marker of oocyte quality
The DCI Paradox
Ovulation Induction
•Higher Pregnancy rates with letrozole in PCOS
•Clear superiority of low dose FSH over CC for first line treatment of Anovulatory PCOS
•With a Starting dose of 75 IU FSH in small in incremental dose rises of not more than ½ the initial dose. 90% will get the criteria for HCG within 14 days
Long term Consequences of PCOS (RCOG 2014)
•GDM
•Type II DM – 5 to 10 times Increased risk 18% to 20 % IGT
•IR
•OSA
•CVS disease / HT / Hyperlipidemia, Metabolic syndrome.
• Endometrial carcinoma - due to unopposed oestrogen stimulation on the endometrium.
•Metabolic syndrome occurring in PCOS is syndrome xx
Thank You !